Process mapping in healthcare: a systematic review
It is so rare to come across a study of process mapping in healthcare (or any Public Sector specific reviews) let alone one so comprehensive as this study. In fact, the research shows there is currently no systematic review of the use of PM in healthcare practice. Most published literature only describes empirical studies of individual interventions using PM.
We have summarised the findings of the report which is based in the healthcare area but we see huge parallels with the wider Public Sector and even private sector organisations. This report is very useful in terms of identifying ways we can improve the way we improve processes and deliver quality improvement and continuous improvement. Process mapping is critical and the report shows us there are currently challenges in the way this is being delivered.
The report reviews a large number of existing studies and has identified a framework for process mapping derived from healthcare, manufacturing and other service industries due to the lack of data and research in just the healthcare arena. The abstract is contained below.
Process mapping (PM) supports a better understanding of complex systems and adaptation of improvement interventions to their local context. However, there is little research on its use in healthcare. This study (i) proposes a conceptual framework outlining quality criteria to guide the effective implementation, evaluation and reporting of PM in healthcare; (ii) reviews published PM cases to identify context and quality of PM application, and the reported benefits of using PM in healthcare.
(bmchealthservres.biomedcentral.com)
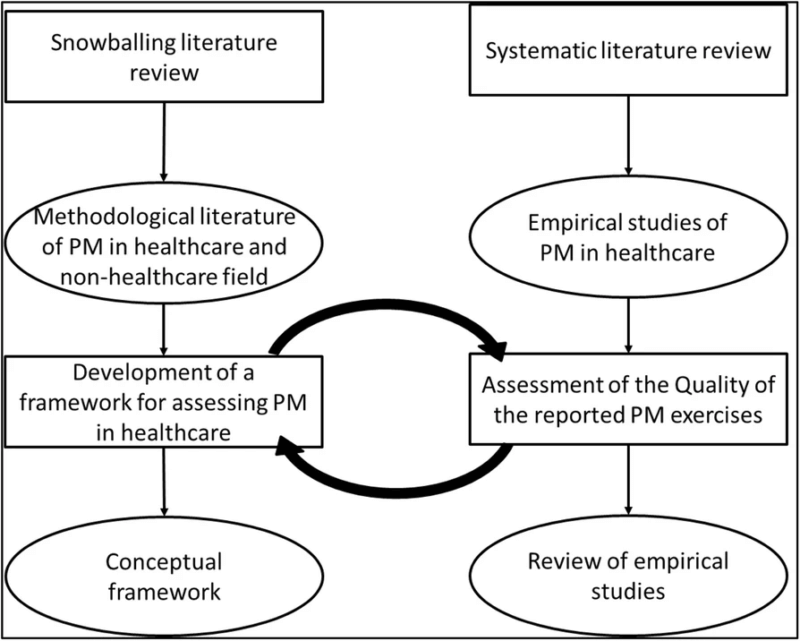
A conceptual framework was identified and then applied to a literature review of empirical studies of process mapping in healthcare. These studies were assessed against the framework as shown in the diagram below.
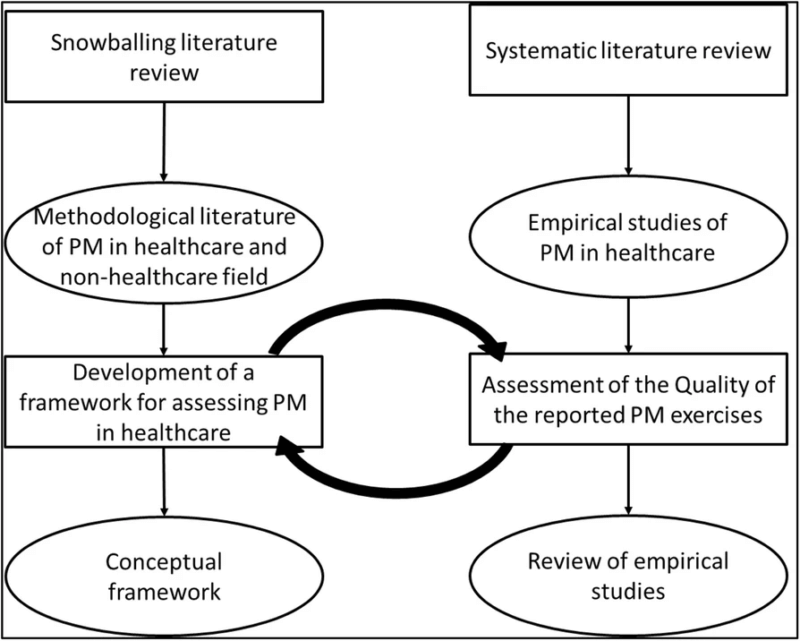
This paper reviews the empirical literature and methodological guidance on PM to increase understanding of its use in healthcare to (1) develop a conceptual framework identifying different phases in PM, with quality criteria for each, to guide the effective implementation, assessment and reporting of this method; (2) identify the context of the use of PM in healthcare QI projects; (3) assess the adherence of the application of PM as described in empirical literature to the proposed conceptual framework quality criteria and (4) explore the reported evidence for the benefits of using PM in improvement work.
(bmchealthservres.biomedcentral.com)
The Conceptual Framework
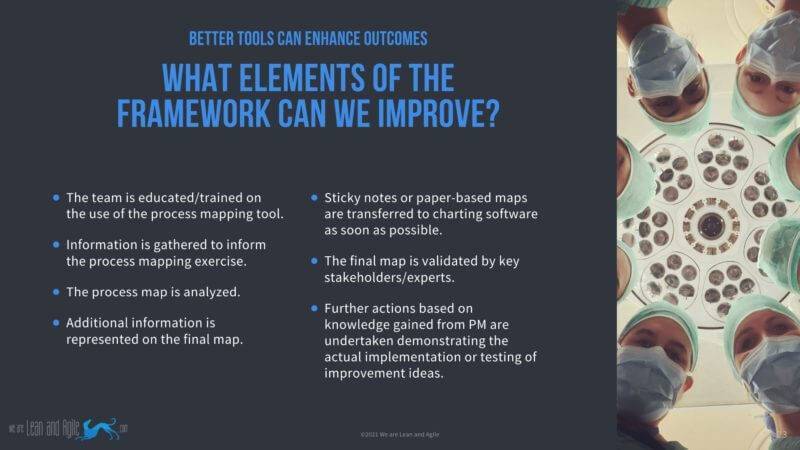
Six studies were identified in the snowballing literature review of methodological publications on PM in healthcare and other service and manufacturing industries to develop the conceptual framework. Through that research, five distinct phases were identified and quality criteria were identified for each individual element. The phases and quality criteria identified are detailed below.
| Phase |
Description |
Quality Criteria |
| 1 |
Preparation, planning and process identification |
A service family and the patient/service user groups are clearly identified. |
|
|
The team is educated/trained on the use of the process mapping tool. |
|
|
A patient representative is involved in the project. |
| 2 |
Data and information gathering |
Information is gathered to inform the process mapping exercise. |
| 3 |
Map generation |
Different perspectives from multiple stakeholders groups are gathered. |
| 4 |
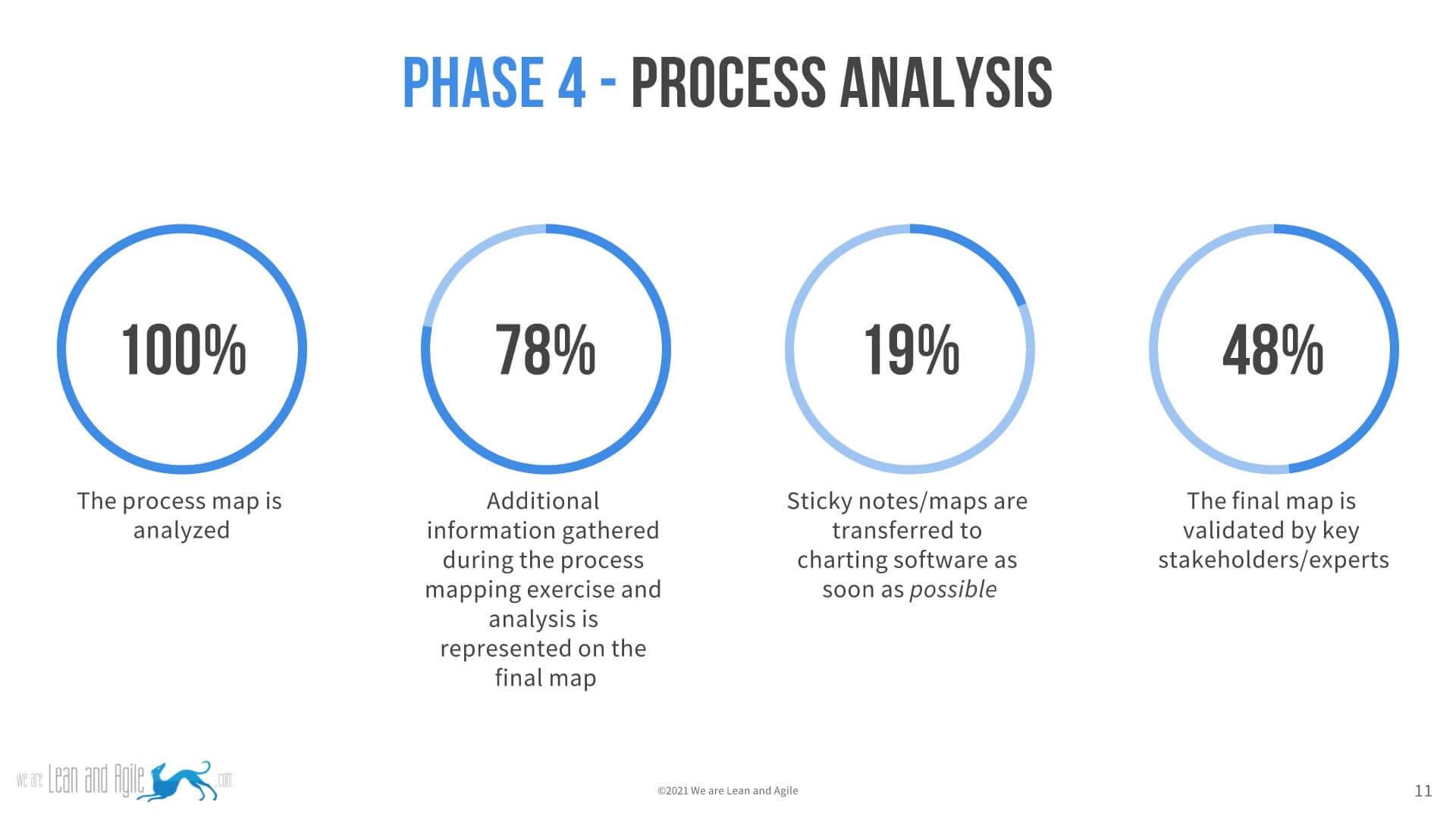
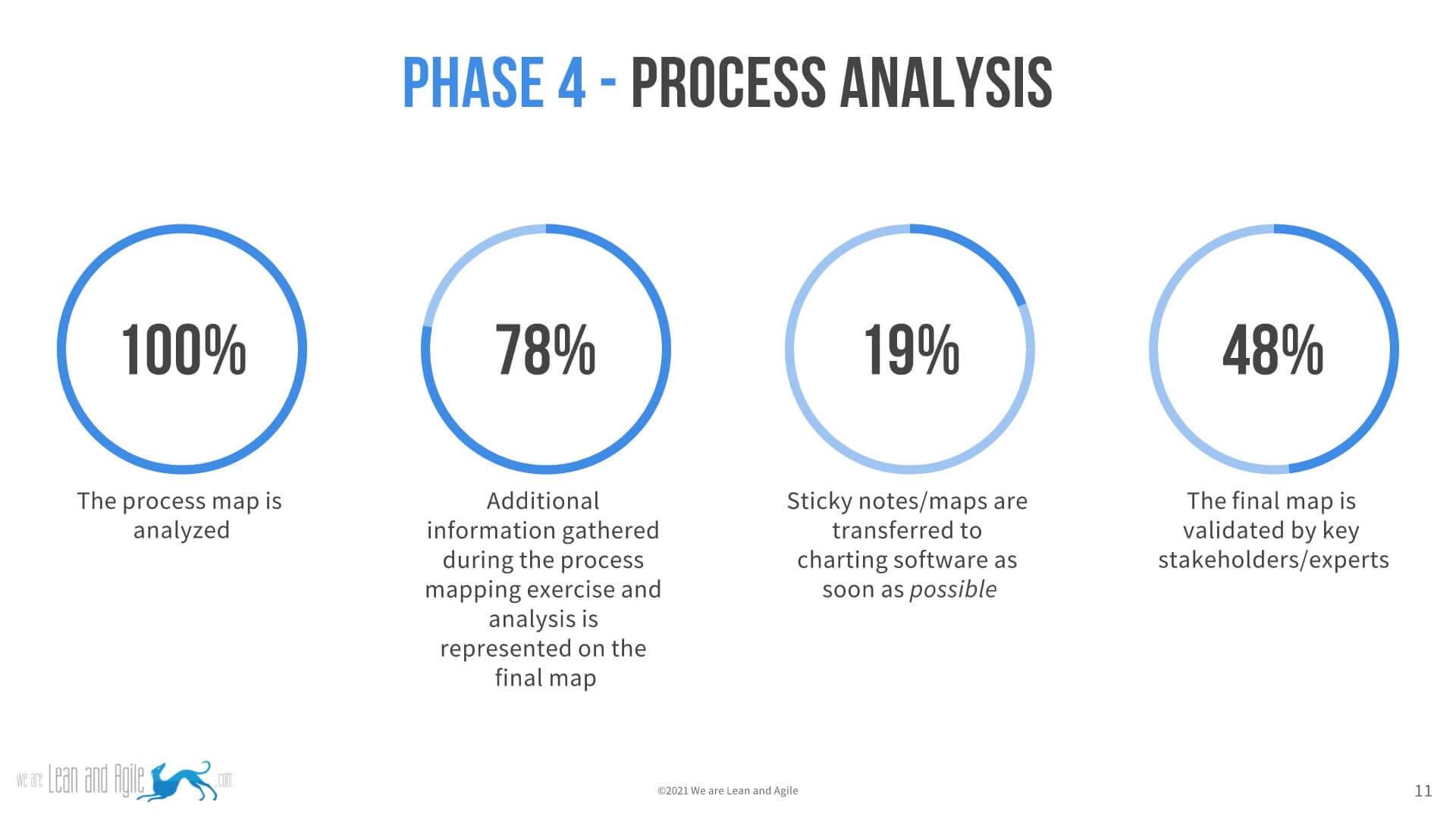
Process analysis |
The process map is analysed. |
|
|
Additional information gathered during the process mapping exercise and analysis is represented on the final map. |
|
|
Sticky notes or paper-based maps are transferred to charting software as soon as possible. |
|
|
The final map is validated by key stakeholders/experts. |
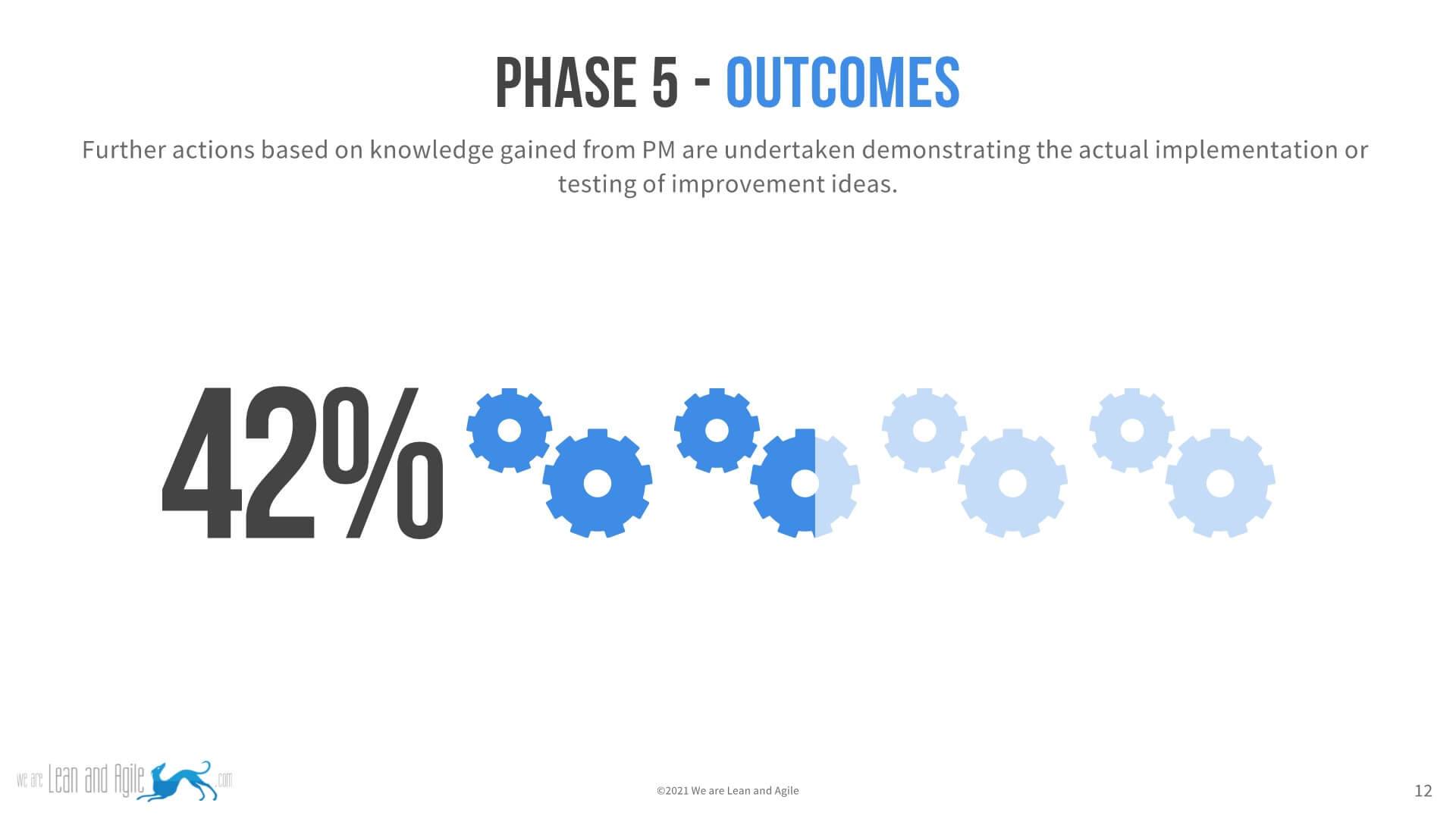
| 5 |
Take it forward |
Further actions based on knowledge gained from PM are undertaken demonstrating the actual implementation or testing of improvement ideas. |
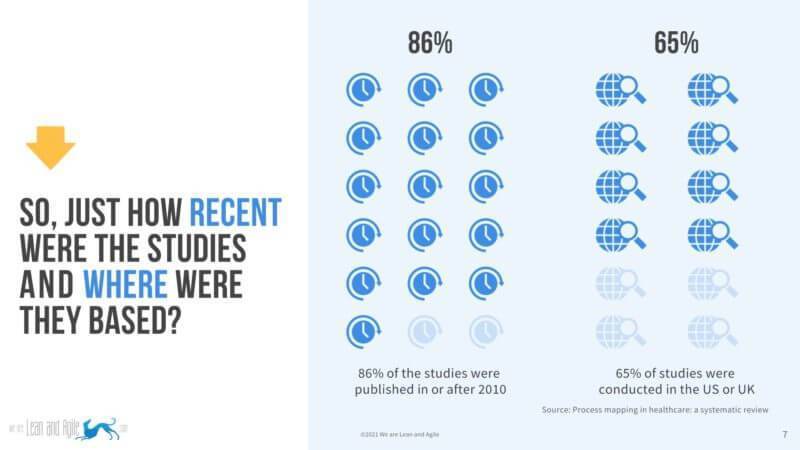
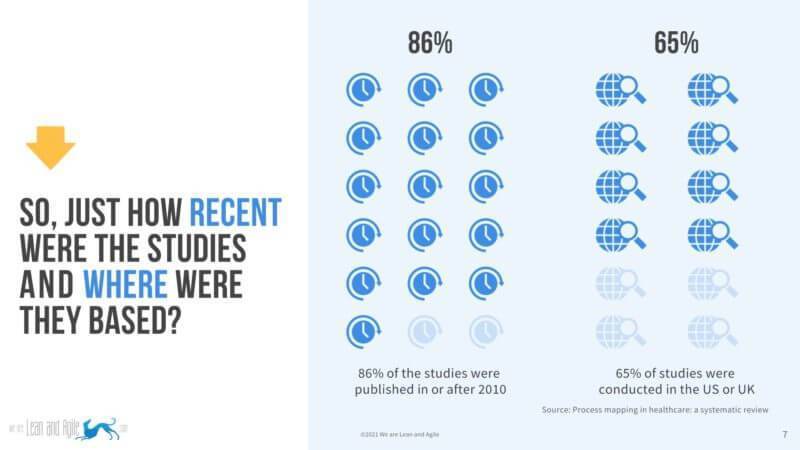
The study data
Over 2500 articles were analysed for their suitability for inclusion in the study and 105 studies met the inclusion criteria identified by the researchers. These 105 articles were then assessed to ascertain their compliance with the conceptual framework.
- The study quality was moderate to high with 94% meeting between eight and ten of the criteria.
- 86% of the studies were from 2010 or later.
- 65% of the studies were conducted in the US or UK
The results of the study
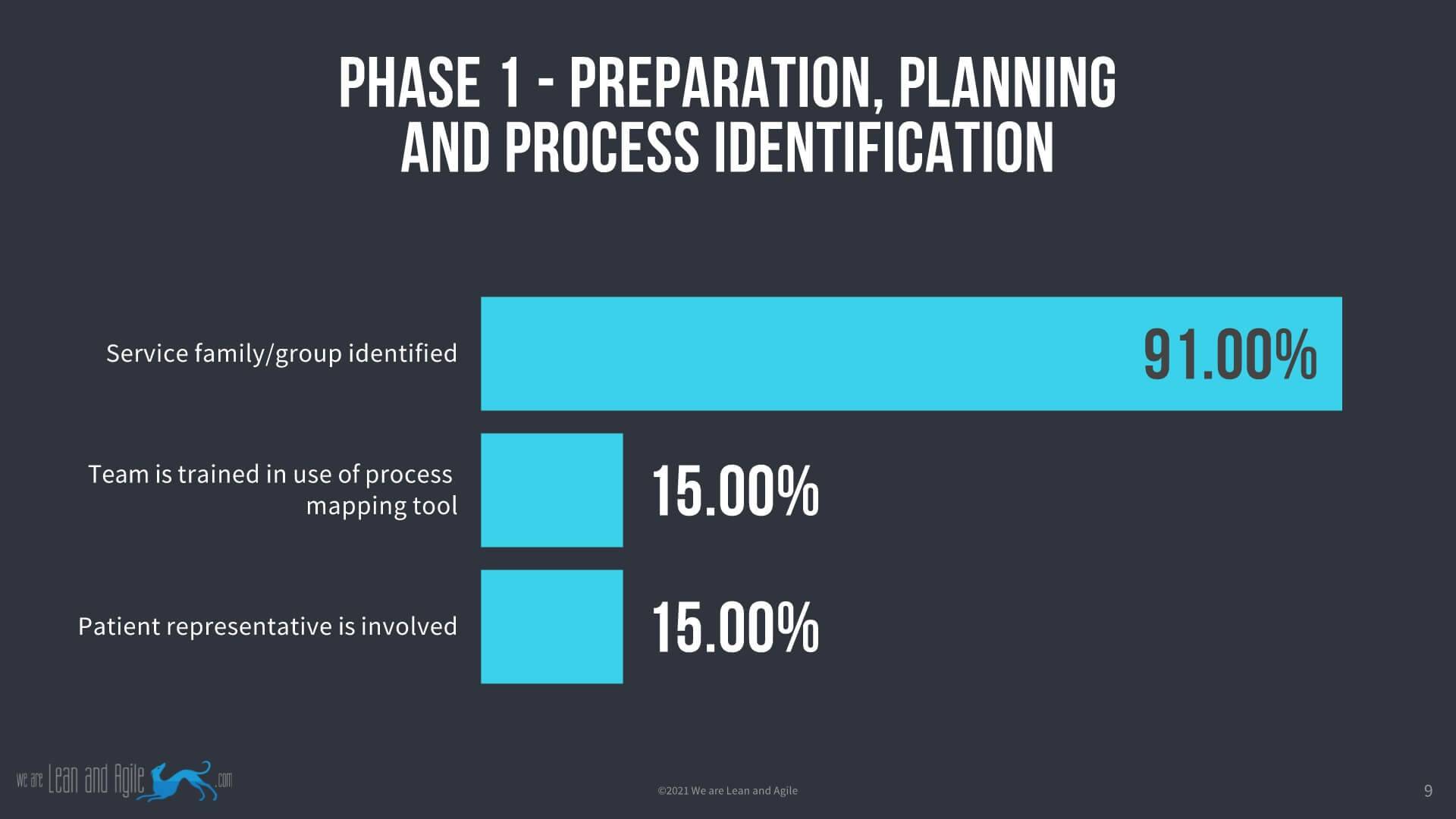
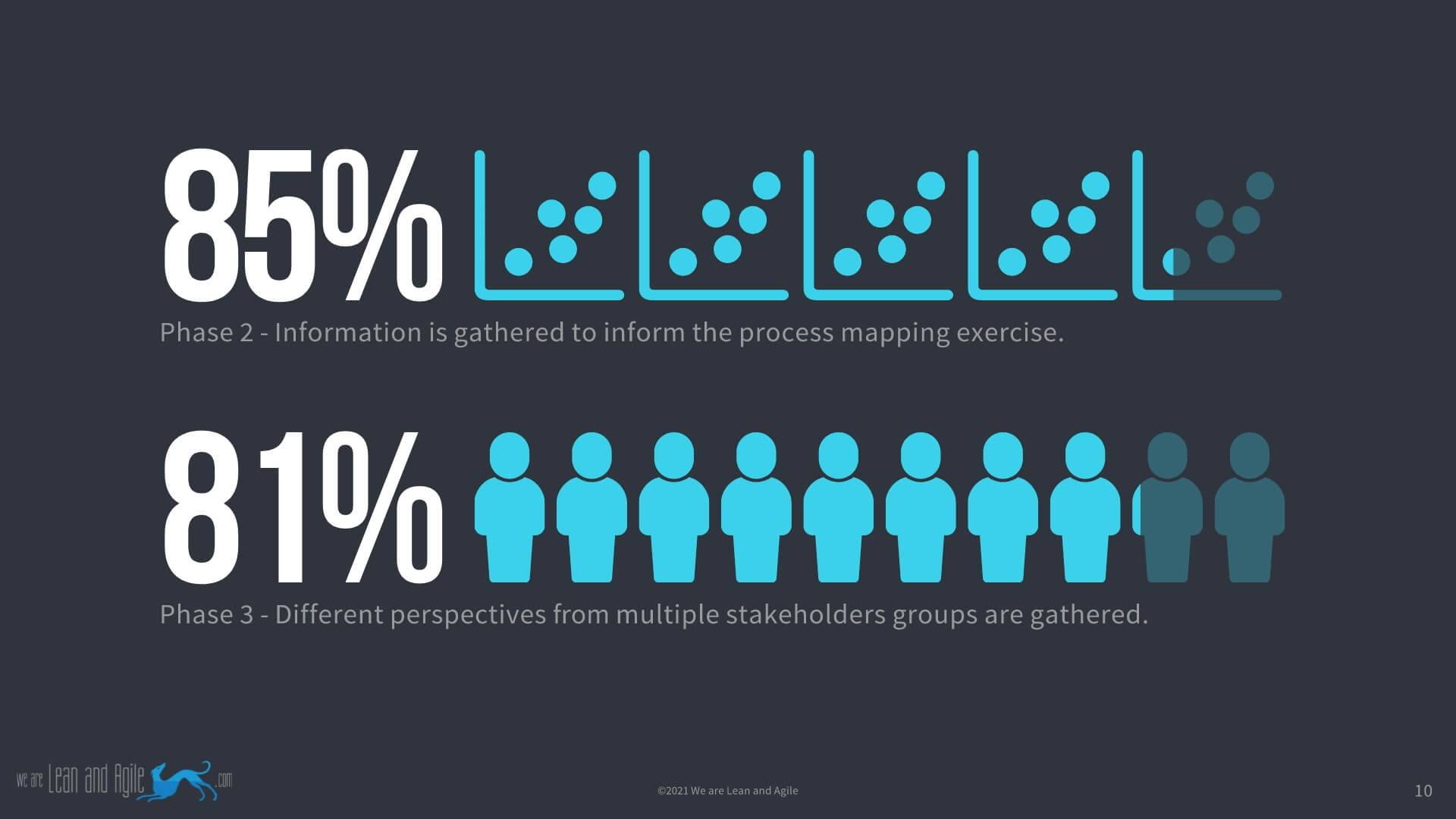
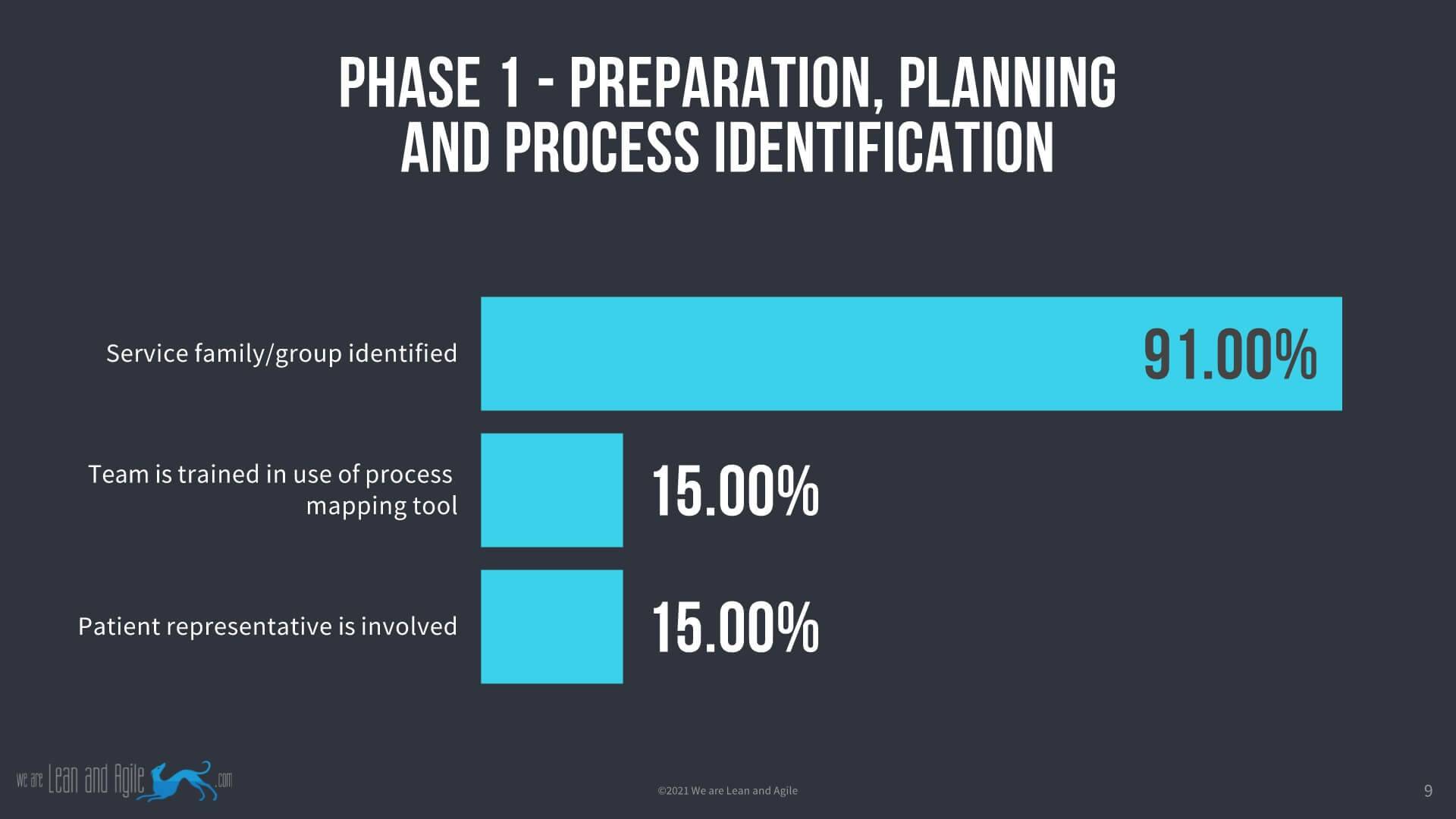
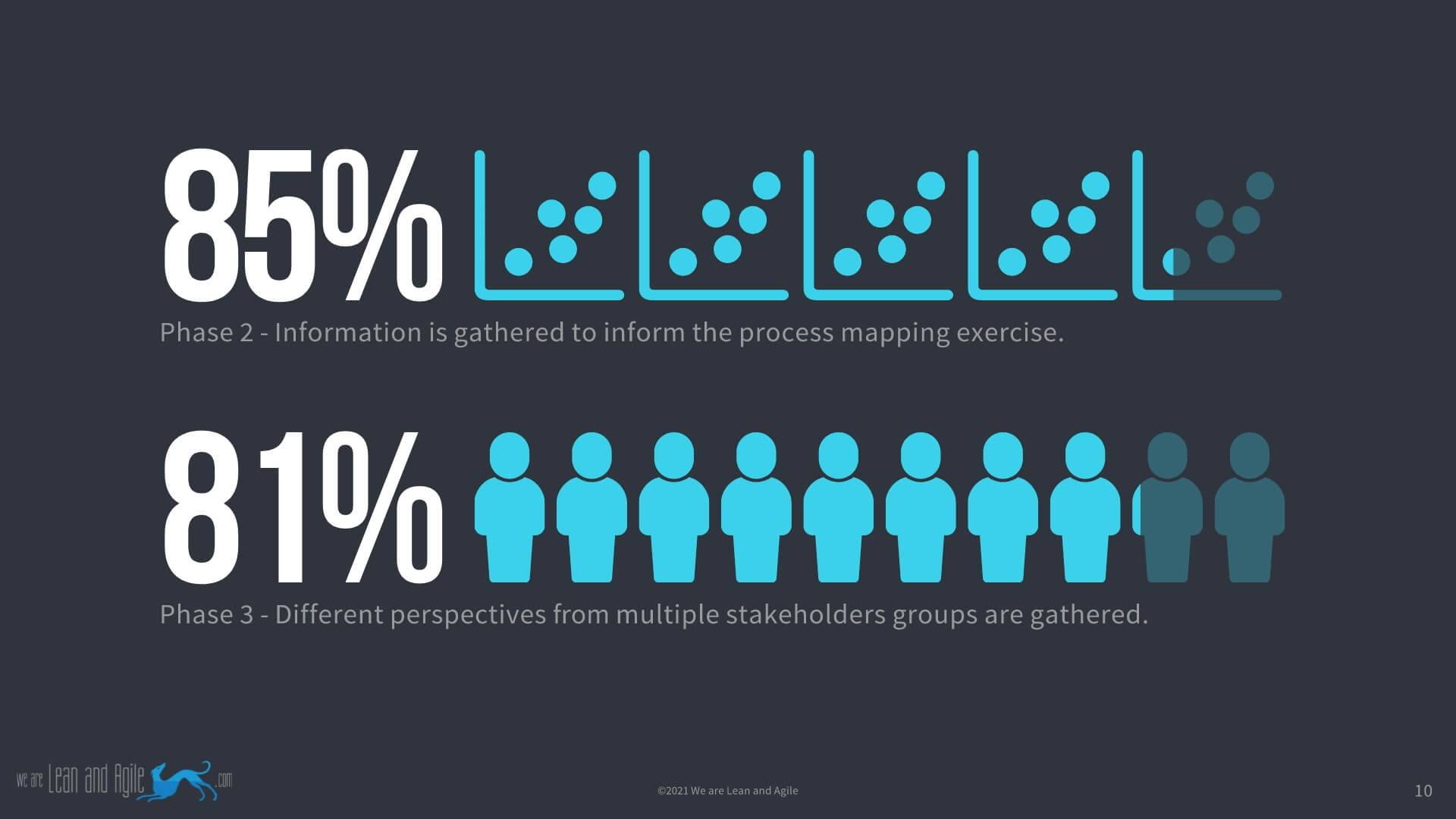
They assessed all empirical studies against the conceptual framework quality criteria for each phase of the 10 elements of the process mapping conceptual framework. The compliance of the studies to the entire framework was quite low as you can see from the image below.

The breakdown of the results by each of the 10 elements is shown in the table below:
| Quality Criteria |
Results (% Compliance) |
| A service family and the patient/service user groups are clearly identified. |
91% |
| The team is educated/trained on the use of the process mapping tool. |
15% |
| A patient representative is involved in the project. |
15% |
| Information is gathered to inform the process mapping exercise. |
85% |
| Different perspectives from multiple stakeholders groups are gathered. |
81% |
| The process map is analysed. |
100% |
| Additional information gathered during the process mapping exercise and analysis is represented on the final map. |
78% |
| Sticky notes or paper-based maps are transferred to charting software as soon as possible. |
19% |
| The final map is validated by key stakeholders/experts. |
48% |
| Further actions based on knowledge gained from PM are undertaken demonstrating the actual implementation or testing of improvement ideas. |
42% |
Please see the actual report for more details of the results. Clearly, this is a literature review with studies not necessarily created to demonstrate process mapping so this can have an impact on the results of the study however the levels of compliance are very low in certain critical areas.
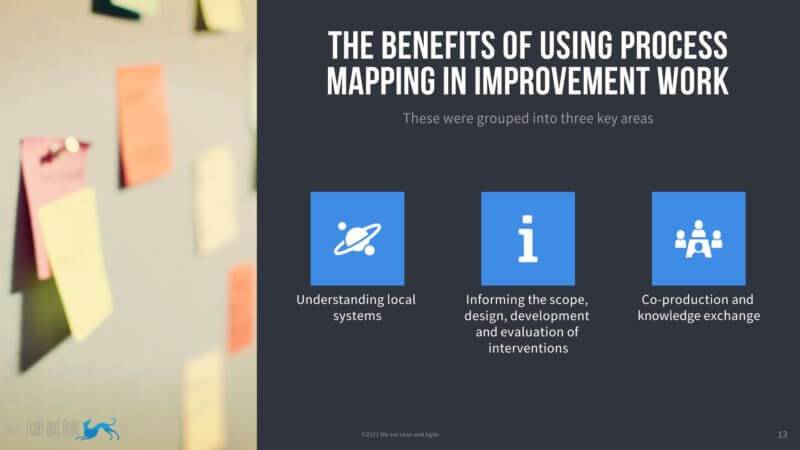
The benefits of using process mapping in improvement work
In the report, the benefits of using process mapping in improvement initiatives were identified as the empirical literature was reviewed. They grouped the benefits into 3 key areas:
- Understanding local systems;
- Informing the scope, design, development and evaluation of interventions;
- Co-production and knowledge exchange;
Below we detail the key benefits identified in each of those areas:
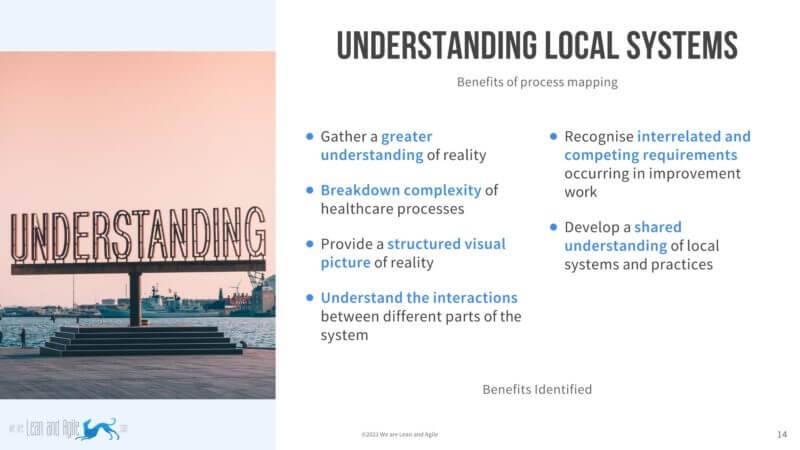
Understanding local systems
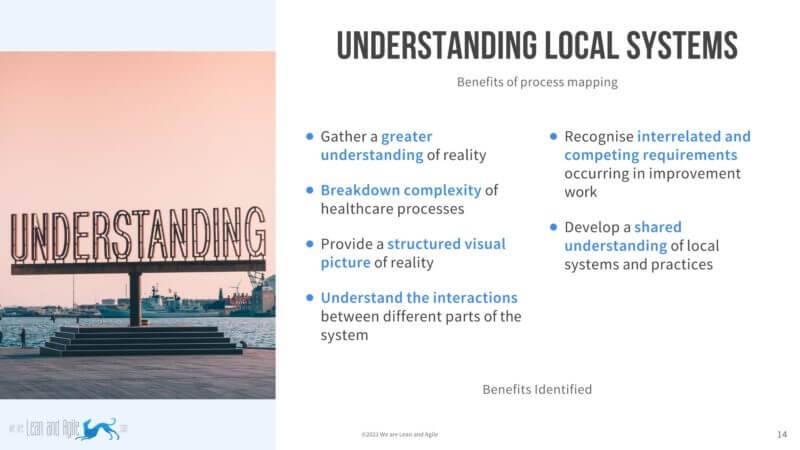
- gather a greater understanding of reality;
- breakdown complexity of healthcare processes;
- provide a structured visual picture of reality;
- understand the interactions between different parts of the system;
- recognise interrelated and competing requirements occurring in improvement work;
- develop a shared understanding of local systems and practices.
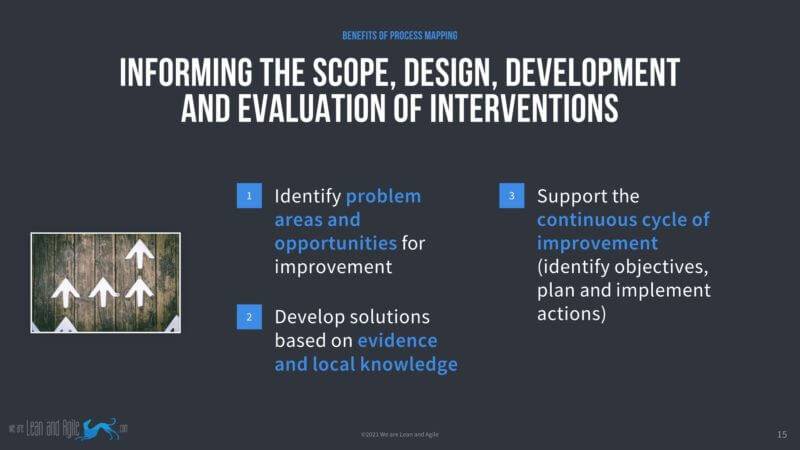
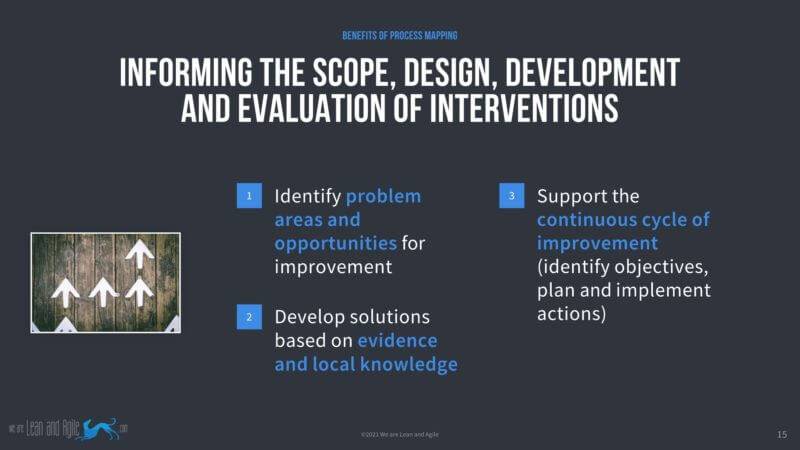
Informing the scope, design, development and evaluation of interventions
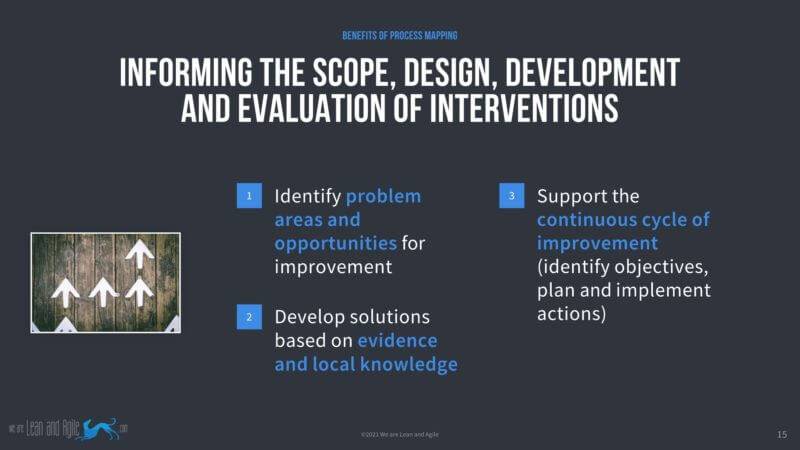
- identify problem areas and opportunities for improvement;
- develop solutions based on evidence and local knowledge;
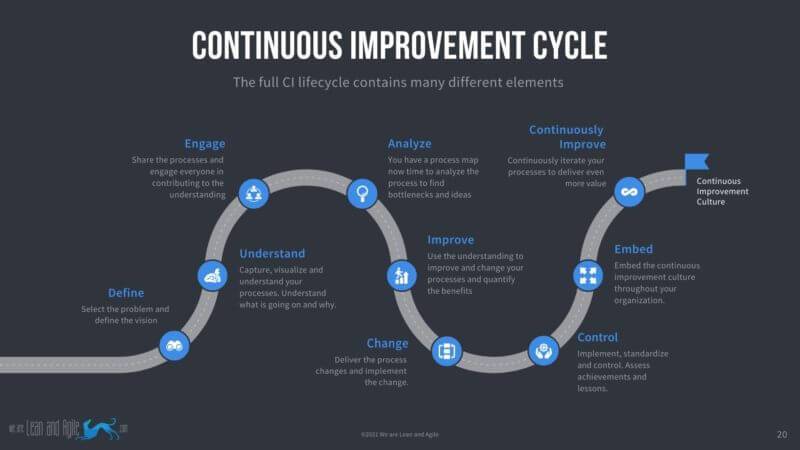
- support the continuous cycle of improvement (identify objectives, plan and implement actions).
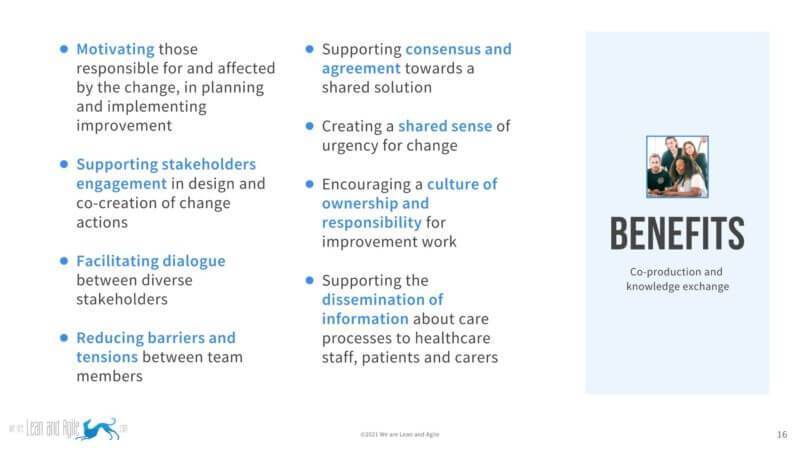
Co-production and knowledge exchange
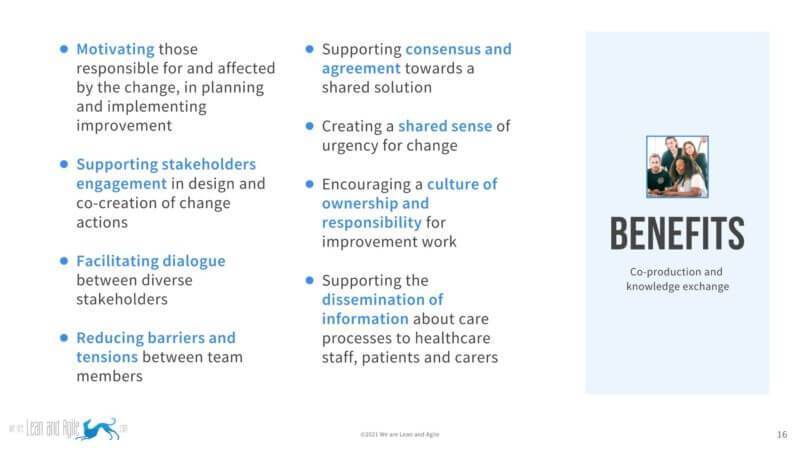
- motivating those responsible for and affected by the change, in planning and implementing improvement:
- supporting stakeholders engagement in design and co-creation of change actions;
- facilitating dialogue between diverse stakeholders;
- reducing barriers and tensions between team members;
- supporting consensus and agreement towards a shared solution;
- creating a shared sense of urgency for change;
- encouraging a culture of ownership and responsibility for improvement work;
- supporting the dissemination of information about care processes to healthcare staff, patients and carers.
Conclusions from the report process mapping in healthcare
This section is taken directly from the
report:
PM is at the heart of a range of different improvement projects in healthcare. Its effective use is often a fundamental component of successful QI initiatives. If appropriately used, PM brings together perspectives of diverse stakeholders to harness tacit knowledge and understand complex processes, as well as to find common solutions and enhance team engagement. However, variance in reporting and lack of compliance with guiding principles underpinning its effective use may inhibit its full potential in healthcare improvement initiatives, and in sharing learning between initiatives. Greater scientific rigor in the application and reporting of PM is required to increase its effectiveness as a method for improvement and advance the field of improvement science.
The conceptual framework proposed in this paper provides generalisable quality criteria to help “unpack the black box” of PM across a variety of settings and problems in healthcare. We encourage the use and further development of these criteria to guide future adoption of PM and for reporting and evaluating its efficacy. A better understanding of the circumstances surrounding decisions about the deployment of mechanisms supporting QI methods, such as PM, is needed in order to increase their effectiveness. Greater recognition of the benefits of PM, as well as training in this method for healthcare professionals and improvement leaders, would also contribute to its more extensive and appropriate use in practice.
Reflections on the results from this report
The report clearly identifies many benefits to process mapping in the NHS and Healthcare. This reflects our experience working in this field in the public and private sectors for 20 years. These benefits can be unlocked by being better at delivering process improvement and quality improvement specifically when it comes to capturing process maps.
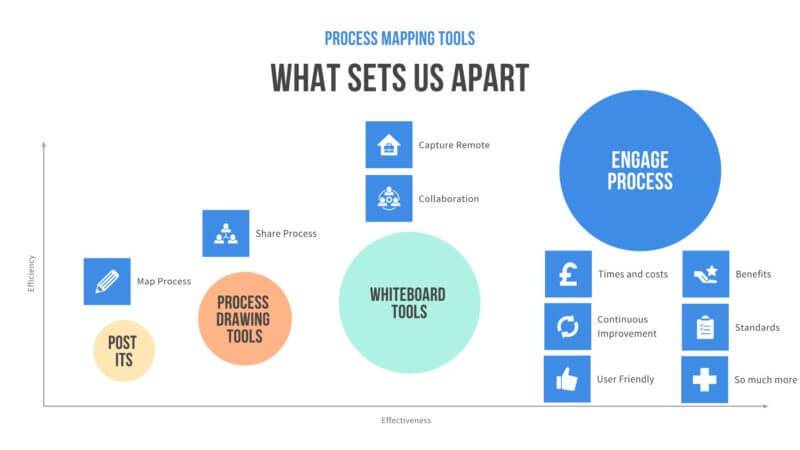
The absence of effective tools does hamper organisations ability to deliver the maximum benefits of service improvement and healthcare improvement projects. But tools do not have to hold you back they can help you deliver your healthcare improvement interventions (in fact whatever sector you work in) even more effectively.
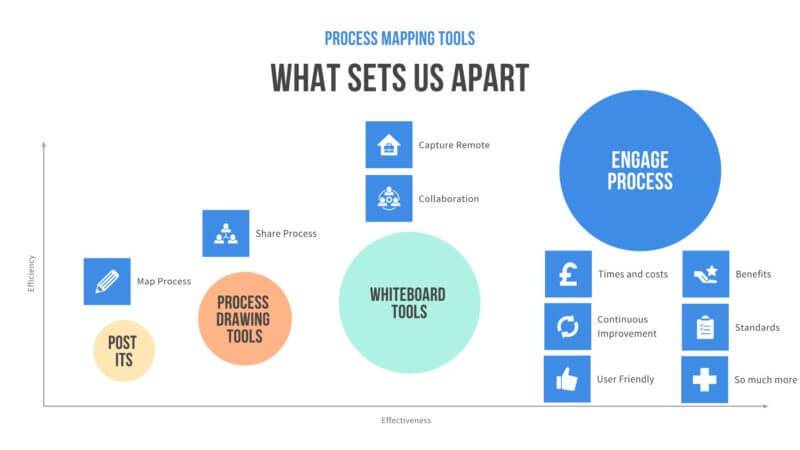
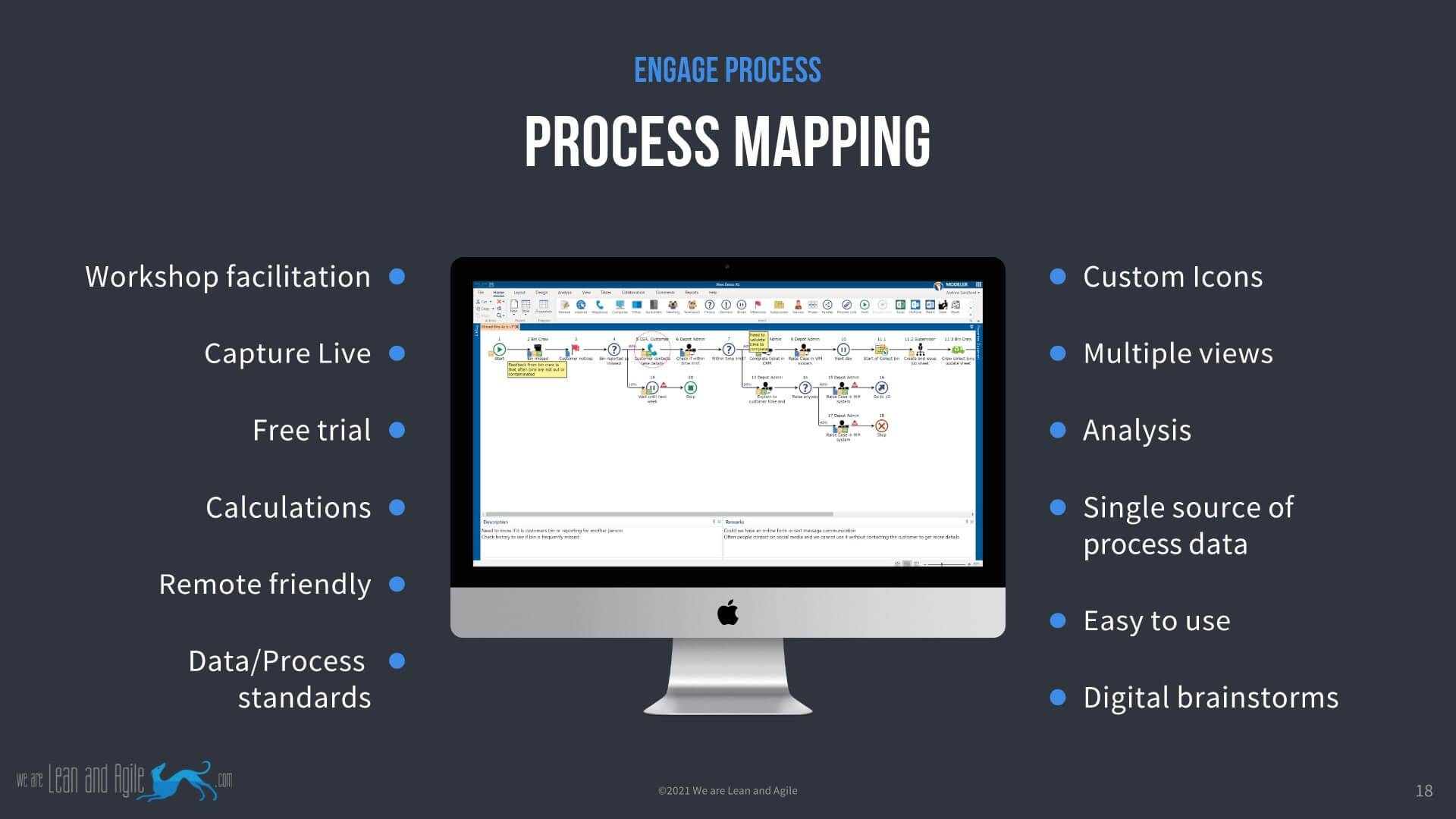
Traditional tools enable you to capture process maps digitally after the workshop and even some whiteboarding tools like Miro or Mural allow you to capture maps live in a workshop. These tools though only give you a picture of a process, not a process model. You cannot capture process metadata so you end up storing information in different places. You certainly cannot calculate costs and times related to your process. This is why we use Engage Process and why we coach and train our users to get the most out of the system just like
Wrexham Council
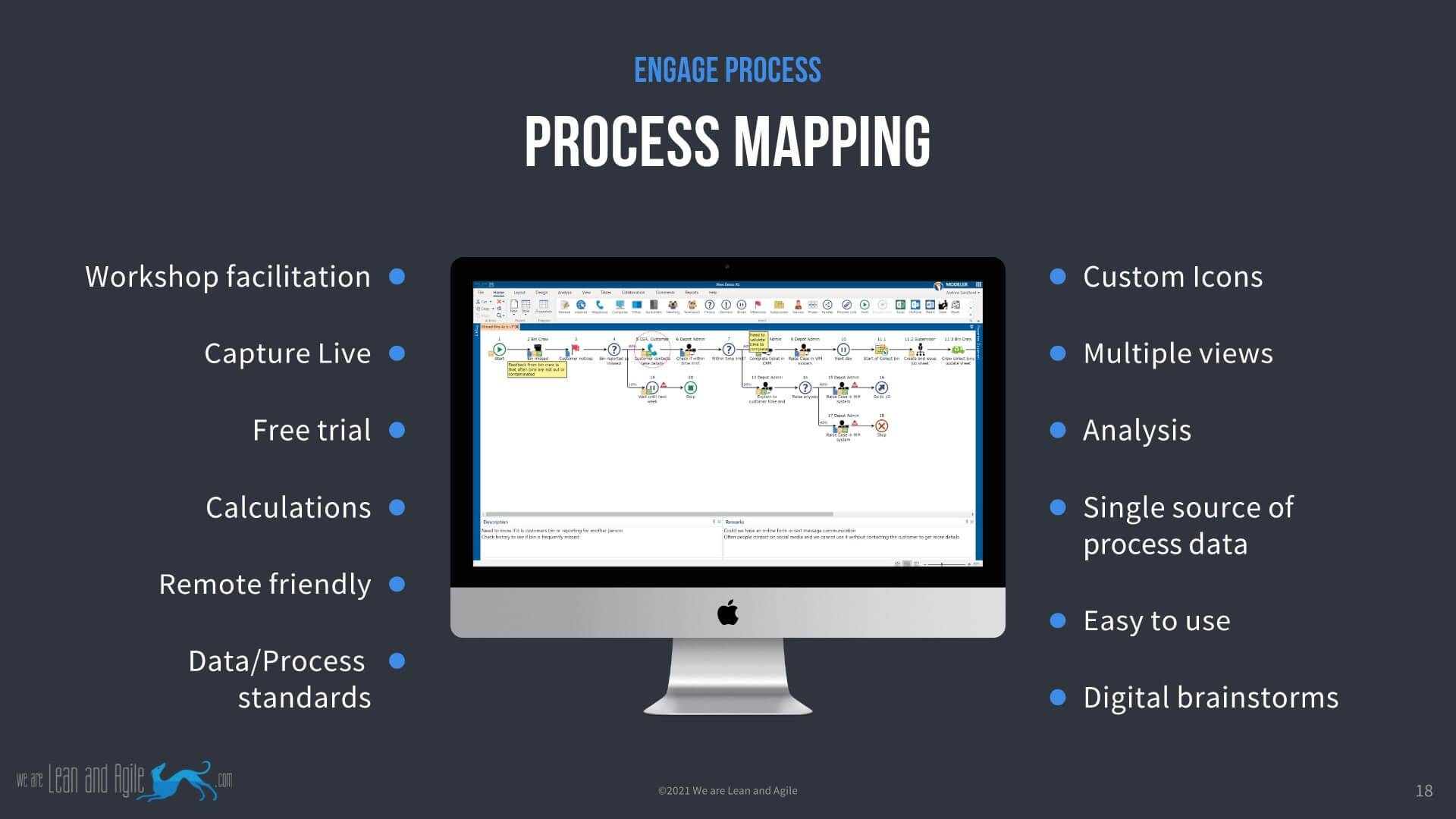
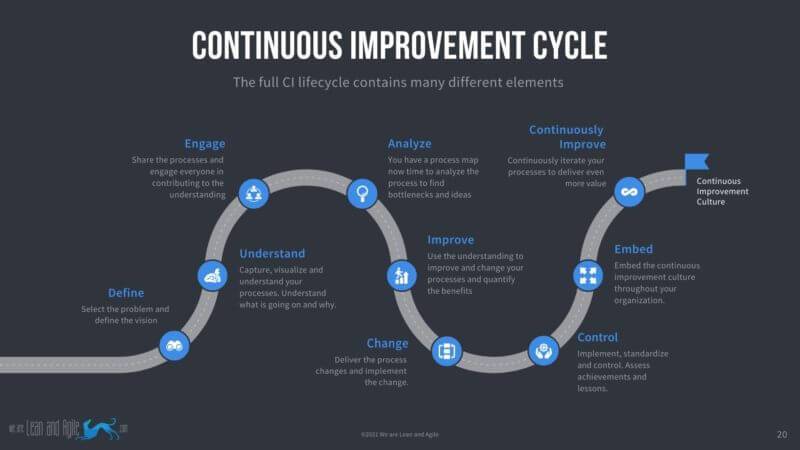
Engage Process helps you to deliver the entire continuous improvement cycle and not only saves your analysts time but helps you to capture, analyse, share, improve, implement and iterate your business processes in a far more efficient and effective way.
The study itself highlights the fact that 100% of studies analysed the process but there is an analysis and then there is analysis. Being able to understand(automatically calculate) the times and the costs related to your process is a real gamechanger in our experience for delivering a successful implementation of improvement projects in healthcare and beyond.
Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.

Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.
Our belief is that Engage Process helps address a number of the elements of the conceptual framework and offers significant benefits over traditional approaches to mapping.
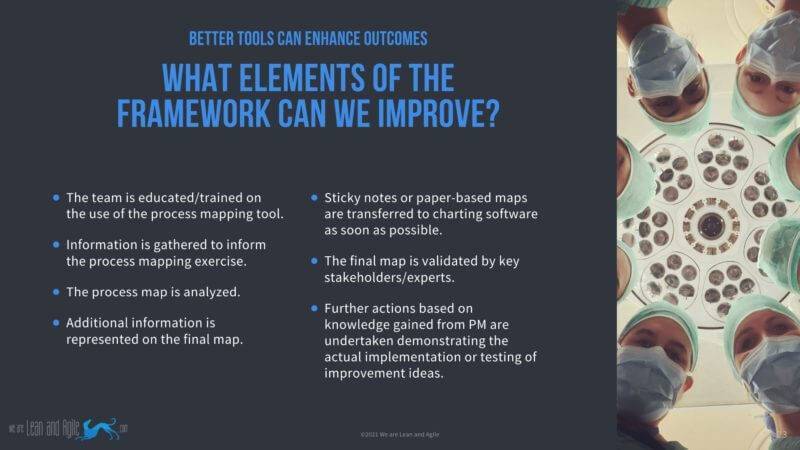
- It helps make it easy to train anyone to deliver high-quality mapping sessions, process maps and outputs
- You capture processes live in the workshops meaning there is no need to transfer to a digital version post-workshop
- Analysis capability and quality of outputs is greatly enhanced by being able to analyse times and costs as well as many other functions not possible in legacy software
- Additional information captured during the exercise is added at the time
- It is easy to add data received post-workshop and to edit the maps
- All data relating to the map can be captured and stored in one place (your process map)
- Maps can be shared digitally and feedback captured and stored against the map
- The likelihood of delivering actions as a result of the map is enhanced by having more data and information to justify and demonstrate your findings
How can you see for yourself?
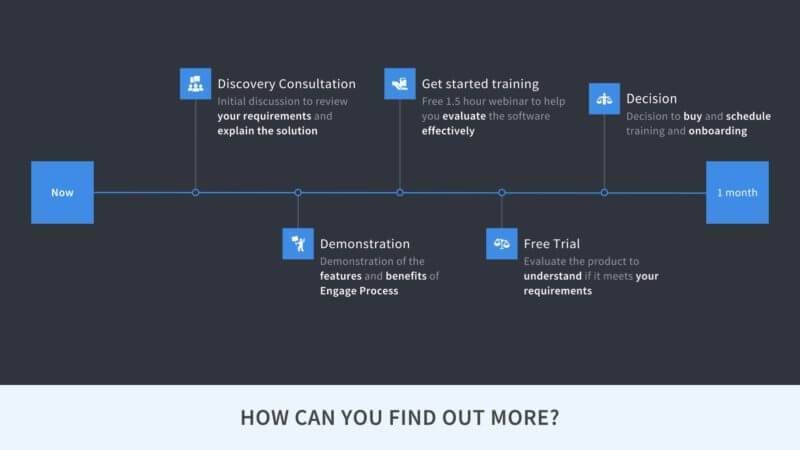
We have been working with many customers in both the public and the private sector for a number of years now. We have developed and iterated an approach to helping our customers evaluate if our solution is right for them. Evaluation does not cost you a penny and is designed to make the evaluation easy for you. The steps are as follows:
- Initial Consultation
- Demonstration to team
- Free trial and training
- Decision to proceed
If you wish to find out more why not book a slot for an initial
15-minute consultation or if you would just like to see some more detail have a look at our
short overview videos here just sign up and watch.
Based on this article
Process mapping in healthcare: a systematic review
BMC Health Services Research volume 21, Article number: 342 (2021)
 This paper reviews the empirical literature and methodological guidance on PM to increase understanding of its use in healthcare to (1) develop a conceptual framework identifying different phases in PM, with quality criteria for each, to guide the effective implementation, assessment and reporting of this method; (2) identify the context of the use of PM in healthcare QI projects; (3) assess the adherence of the application of PM as described in empirical literature to the proposed conceptual framework quality criteria and (4) explore the reported evidence for the benefits of using PM in improvement work. (bmchealthservres.biomedcentral.com)
This paper reviews the empirical literature and methodological guidance on PM to increase understanding of its use in healthcare to (1) develop a conceptual framework identifying different phases in PM, with quality criteria for each, to guide the effective implementation, assessment and reporting of this method; (2) identify the context of the use of PM in healthcare QI projects; (3) assess the adherence of the application of PM as described in empirical literature to the proposed conceptual framework quality criteria and (4) explore the reported evidence for the benefits of using PM in improvement work. (bmchealthservres.biomedcentral.com)
 The breakdown of the results by each of the 10 elements is shown in the table below:
The breakdown of the results by each of the 10 elements is shown in the table below:
 In the report, the benefits of using process mapping in improvement initiatives were identified as the empirical literature was reviewed. They grouped the benefits into 3 key areas:
In the report, the benefits of using process mapping in improvement initiatives were identified as the empirical literature was reviewed. They grouped the benefits into 3 key areas:
 The report clearly identifies many benefits to process mapping in the NHS and Healthcare. This reflects our experience working in this field in the public and private sectors for 20 years. These benefits can be unlocked by being better at delivering process improvement and quality improvement specifically when it comes to capturing process maps.
The absence of effective tools does hamper organisations ability to deliver the maximum benefits of service improvement and healthcare improvement projects. But tools do not have to hold you back they can help you deliver your healthcare improvement interventions (in fact whatever sector you work in) even more effectively.
The report clearly identifies many benefits to process mapping in the NHS and Healthcare. This reflects our experience working in this field in the public and private sectors for 20 years. These benefits can be unlocked by being better at delivering process improvement and quality improvement specifically when it comes to capturing process maps.
The absence of effective tools does hamper organisations ability to deliver the maximum benefits of service improvement and healthcare improvement projects. But tools do not have to hold you back they can help you deliver your healthcare improvement interventions (in fact whatever sector you work in) even more effectively.
 Traditional tools enable you to capture process maps digitally after the workshop and even some whiteboarding tools like Miro or Mural allow you to capture maps live in a workshop. These tools though only give you a picture of a process, not a process model. You cannot capture process metadata so you end up storing information in different places. You certainly cannot calculate costs and times related to your process. This is why we use Engage Process and why we coach and train our users to get the most out of the system just like Wrexham Council
Traditional tools enable you to capture process maps digitally after the workshop and even some whiteboarding tools like Miro or Mural allow you to capture maps live in a workshop. These tools though only give you a picture of a process, not a process model. You cannot capture process metadata so you end up storing information in different places. You certainly cannot calculate costs and times related to your process. This is why we use Engage Process and why we coach and train our users to get the most out of the system just like Wrexham Council
 Engage Process helps you to deliver the entire continuous improvement cycle and not only saves your analysts time but helps you to capture, analyse, share, improve, implement and iterate your business processes in a far more efficient and effective way.
Engage Process helps you to deliver the entire continuous improvement cycle and not only saves your analysts time but helps you to capture, analyse, share, improve, implement and iterate your business processes in a far more efficient and effective way.
 The study itself highlights the fact that 100% of studies analysed the process but there is an analysis and then there is analysis. Being able to understand(automatically calculate) the times and the costs related to your process is a real gamechanger in our experience for delivering a successful implementation of improvement projects in healthcare and beyond.
Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.
The study itself highlights the fact that 100% of studies analysed the process but there is an analysis and then there is analysis. Being able to understand(automatically calculate) the times and the costs related to your process is a real gamechanger in our experience for delivering a successful implementation of improvement projects in healthcare and beyond.
Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.
 Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.
Our belief is that Engage Process helps address a number of the elements of the conceptual framework and offers significant benefits over traditional approaches to mapping.
Our software also helps by introducing standards over the way you map and the data you capture based on BPNM but with user-friendly visual icons. And in terms of writing up the outputs of workshops, you can have all that time back when you capture live in the workshops. This also helps the stakeholders as the map they saw in the workshop is the map they get back. This helps break down the complexity of process management for the stakeholders.
Our belief is that Engage Process helps address a number of the elements of the conceptual framework and offers significant benefits over traditional approaches to mapping.
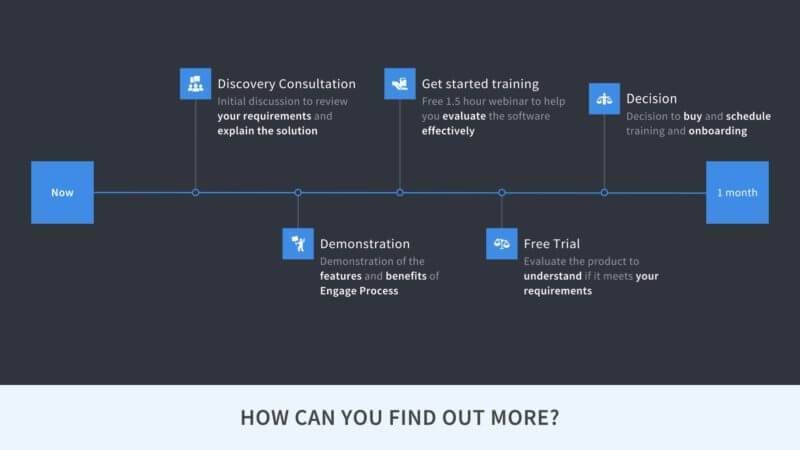 We have been working with many customers in both the public and the private sector for a number of years now. We have developed and iterated an approach to helping our customers evaluate if our solution is right for them. Evaluation does not cost you a penny and is designed to make the evaluation easy for you. The steps are as follows:
We have been working with many customers in both the public and the private sector for a number of years now. We have developed and iterated an approach to helping our customers evaluate if our solution is right for them. Evaluation does not cost you a penny and is designed to make the evaluation easy for you. The steps are as follows:
